A 56yr old man with generalized lymphadenopathy
FINAL EXAMINATION CASE REPORT
NAME: Meghana.M
Hall ticket no: 1701006118
Batch: 2017
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box"
CASE PRESENTATION :
HISTORY :
A 56 year old male patient, daily wage worker by occupation, resident of Nalgonda came to opd with
CHIEF COMPLAINTS :
1. Pain abdomen since 20 days.
2. Multiple abdominal swellings since 7 days.
3. Fever since 7 days
HISTORY OF PRESENT ILLNESS :
Patient was apparently asymptomatic 5 months back, then he developed Dry cough which was insidious in onset, gradually progressive and there was no sputum. Later, he developed fever which was high grade, associated with chills and rigors. He went to the hospital with above complaints and medications were prescribed and the symptoms subsided.
After 2 months, patient observed loss of weight and loss of appetite for which he went to the doctor. Upon, his advice, the patient got tested for Tuberculosis and HIV. He tested positive for both TB and HIV. The patient was given ART and ATT.
20 days back, patient started experiencing
- Pain around the umbilicus which was insidious in onset gradually progressive associated with abdominal discomfort.
- Patient also complains of small multiple swellings in the abdomen since 7 days which hav gradually increased to present size.
- He had fever since 7 days, high grade associated with chills and rigors.
PAST HISTORY :
Patient is a known case of Tuberculosis and HIV-AIDS and is on regular treatment.
Patient is not a known case of Diabetes mellitus, Hypertension, Asthma, Epilepsy, Thyroid disorders.
There is no surgical history, no history of blood transfusions.
TREATMENT HISTORY:
PERSONAL HISTORY :
Diet : Mixed
Appetite : Decreased
Sleep : Adequate
Bowel and Bladder movements : Regular
Addictions : None
FAMILY HISTORY :
No history of similar complaints in the family.
HISTORY OF ALLERGIES :
No known drug or food allergies.
GENERAL PHYSICAL EXAMINATION :
Patient is conscious, coherent, co-operative and well oriented to time, place and person.
Moderately built and moderately nourished.
LYMPH NODE EXAMINATION:
Lymphadenopathy is present. There are multiple enlarged lymph nodes in abdomen and neck.
Cervical lymph nodes:
Right side--
Level 5 nodes are positive - lymph nodes in the posterior triangle of neck
3×2cm, mobile, soft to firm in consistency, non matted
Left side--
Level 4 lymph nodes- lower jugular lymph nodes are positive
2×1cm, mobile, soft in consistency, non matted
Inguinal lymph nodes:
Right side--
Right inguinal lymph nodes positive
2-3 in number, 1×1 cm, soft, non tender
Left side--
Left inguinal lymph nodes positive,
3-4 in number, 1×1cm, soft, non tender
Axillary nodes are not palpable.
Vitals :
Temperature : Afebrile
Pulse Rate : 86 bpm
Blood Pressure : 120/80 mm Hg
Respiratory rate : 16 cpm
GRBS : 106 mg/dl
SYSTEMIC EXAMINATION :
Cardiovascular System : S1, S2 heard. No murmurs.
Respiratory System : Normal Vesicular Breath Sounds heard.
Central Nervous System : Conscious, Alert, Speech normal, Motor and Sensory examination normal.
Per Abdomen : Soft. No hepatomegaly. No splenomegaly.
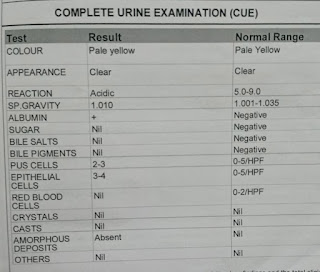
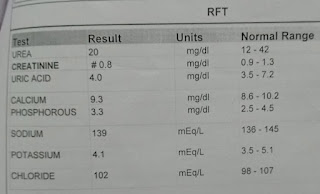
INVESTIGATIONS :
ECG report:
Chest x-ray
2D Echo
FNAC : From right cervical lymph node - acid fast bacilli positive
PROVISIONAL DIAGNOSIS :
Fever with generalized lymphadenopathy secondary to HIV/TB
TREATMENT :
1. Tab. Dolo 650 PO TID
2. Tab. MVT OD
3. Inj. Neomol 1g IV/SOS
4. Tab. Dolutegravir, Lamivudine, Tenofovir Disoproxil Funerate (50 mg,300 mg,300 mg) PO OD
5. Tab. Rifampicin, Isoniazid, Pyrazinamide, Ethambutol (150 mg,75 mg,400 mg,275 mg) PO OD
6. Tab. Septran-DS PO BD
7. Tab. Pan 40 mg PO BD
8. Syrup Aristozyme PO 10 ml TID

























Comments
Post a Comment